“Understanding Heart Valve Disease: Types, Causes, Symptoms, Diagnosis, and Treatment”
Heart Valve Disease: Understanding, Types, Causes, Symptoms, Diagnosis, and Treatment
Heart valve disease is a condition characterized by the improper functioning of the heart valves, vital components that regulate blood flow within the heart. These valves ensure one-way blood flow through the heart, preventing backward leakage and maintaining a continuous circulation. Understanding how heart valves work is essential in grasping the intricacies of this condition.
How Heart Valves Work
Situated at the exit of each heart chamber, heart valves play a crucial role in the cardiac cycle. Blood flows from the atria into the ventricles through the tricuspid and mitral valves. When the ventricles are full, these valves shut to prevent backward blood flow during contraction. Simultaneously, the pulmonic and aortic valves open, allowing blood to be pumped out of the ventricles to the pulmonary artery and aorta, respectively. As the ventricles relax, the aortic and pulmonic valves close, preventing blood from flowing back into the ventricles. This orchestrated sequence repeats with every heartbeat, ensuring continuous blood flow to the heart, lungs, and body.
Types of Heart Valve Disease
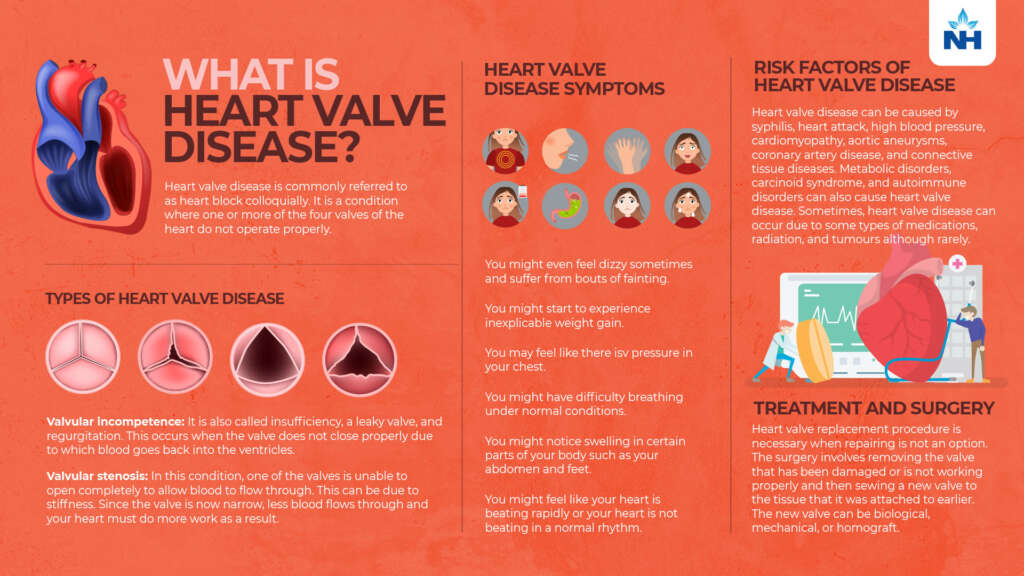
Heart valve disease encompasses various types, broadly categorized into valvular stenosis and valvular insufficiency.
- Valvular Stenosis: Occurs when a valve doesn’t fully open, making the heart work harder to pump blood through. Stenosis can affect any of the four valves, resulting in tricuspid stenosis, pulmonic stenosis, mitral stenosis, or aortic stenosis.
- Valvular Insufficiency: Also known as regurgitation, this condition arises when a valve fails to close tightly, causing blood to leak backward. Depending on the affected valve, it can be termed tricuspid regurgitation, pulmonary regurgitation, mitral regurgitation, or aortic regurgitation.
Causes of Heart Valve Disease
Heart valve disease can be congenital, developing before birth, or acquired later in life. Congenital valve disease often affects the aortic or pulmonic valve, presenting issues like wrong-sized valves or malformed leaflets. Acquired valve disease may result from structural changes due to diseases such as rheumatic fever or endocarditis.
- Rheumatic Fever: Caused by untreated bacterial infections, usually strep throat, it can lead to inflammation of the heart valves, with symptoms appearing years later.
- Endocarditis: Germs entering the bloodstream attack heart valves, causing growths, holes, and scarring. Individuals with valve disease are at a higher risk of endocarditis.
Other causes include coronary artery disease, heart attack, cardiomyopathy, syphilis, high blood pressure, aortic aneurysms, connective tissue diseases, tumors, certain drugs, and radiation.
Symptoms of Heart Valve Disease
Symptoms may vary, but common indications include:
- Shortness of Breath: Particularly during physical activity or while lying down.
- Weakness or Dizziness: Feeling too weak to perform daily activities, with potential episodes of dizziness or fainting.
- Chest Discomfort: Pressure or weight in the chest, especially during activity or exposure to cold air.
- Palpitations: Irregular heart rhythms, skipped beats, or a fluttering sensation in the chest.
- Swelling: Edema in ankles, feet, or abdomen, leading to a bloated feeling.
- Rapid Weight Gain: Significant weight gain within a short timeframe.
Symptoms may not always correlate with the severity of the condition, highlighting the importance of proper diagnosis.
Diagnosis of Heart Valve Disease
Heart valve disease can be diagnosed through a combination of patient history, physical examinations, and diagnostic tests. Techniques such as echocardiography, transesophageal echocardiography, and cardiac catheterization provide detailed insights into valve structure and functionality. Regular monitoring helps track disease progression, guiding treatment decisions.
Treatment Options for Heart Valve Disease
Treatment goals include protecting valves from further damage, alleviating symptoms, and repairing or replacing valves. Strategies involve:
- Protection from Further Damage: Patients, especially those with surgically repaired or replaced valves, must take precautions against endocarditis. This includes informing healthcare providers about valve disease, regular dental care, and antibiotic prophylaxis for certain procedures.
- Medications: Prescribed to manage symptoms and prevent further damage. Common drugs include diuretics, anti-arrhythmics, vasodilators, ACE inhibitors, beta-blockers, and anticoagulants.
- Surgery and Procedures: Surgical interventions, such as heart valve repair or replacement, aim to address structural issues. Traditional and minimally invasive surgeries offer options based on patient characteristics and disease severity.
- Non-surgical Interventions: Percutaneous balloon valvuloplasty and transcatheter aortic valve replacement (TAVR) provide alternative approaches for specific cases.
Living With Heart Valve Disease
Maintaining a healthy lifestyle is crucial for individuals with heart valve disease. Key aspects include:
- Awareness: Understanding the type and extent of valve disease.
- Communication: Informing all healthcare providers about the condition.
- Vigilance: Seeking prompt medical attention for potential infections.
- Oral Health: Maintaining good dental hygiene and regular dental check-ups.
- Medication Adherence: Following prescribed drug regimens and staying informed about their purpose and timing.
- Regular Medical Follow-ups: Scheduled visits to monitor heart health, even in the absence of symptoms.
In conclusion, heart valve disease demands a comprehensive approach, involving awareness, proactive healthcare, and adherence to medical recommendations. By understanding the intricacies of this condition, individuals can actively contribute to their well-being and enhance their quality of life.