Share This Article
Hyperemesis gravidarum, severe nausea and vomiting in the first trimester, is a challenging condition that affects pregnant individuals. This article explores the causes, symptoms, management, and coping strategies for those grappling with this intense morning sickness.
Pregnancy is a time of anticipation and joy, but for some expectant mothers, it can also bring an overwhelming and debilitating challenge: hyperemesis gravidarum. Unlike typical morning sickness, this severe condition leads to relentless nausea and vomiting during the first trimester, potentially leading to dehydration, weight loss, and other complications. Hyperemesis gravidarum can significantly impact a woman’s daily life and well-being. In this guide, we will navigate the complexities of hyperemesis gravidarum. We will provide insights into its causes, symptoms, and consequences. Additionally, we’ll discuss strategies and medical interventions to assist expectant mothers in coping with this challenging condition. This will help safeguard their health and the health of their growing baby.
1.Understanding Hyperemesis Gravidarum
a. Defining Hyperemesis Gravidarum
Hyperemesis Gravidarum (HG) is a severe form of nausea and vomiting during pregnancy that extends beyond the typical morning sickness. It often leads to dehydration, weight loss, and nutritional deficiencies, posing risks to both the pregnant individual and the developing fetus.
b. Causes and Triggers
The exact cause of HG is not fully understood, but hormonal changes, particularly elevated levels of human chorionic gonadotropin (hCG), are believed to contribute. Other factors, like a history of HG in previous pregnancies, multiple gestations (twins or more), and pre-existing conditions, may increase the likelihood of experiencing severe nausea.
Also read: Pregnancy Hormones: Its Role And Effects On Your Body
2. Recognizing the Symptoms
a. Severe Nausea and Unrelenting Vomiting
Individuals with HG experience persistent and severe nausea that goes beyond the typical morning sickness. Vomiting can be frequent and debilitating, occurring multiple times a day. The severity of symptoms can lead to dehydration, electrolyte imbalances, and weight loss.
b. Associated Signs and Complications
In addition to nausea and vomiting, HG may present with other signs such as dizziness, fainting, and ketosis (a condition where the body burns fat for energy). Complications can include nutritional deficiencies, electrolyte imbalances, and, in severe cases, damage to the liver and kidneys.
3. Seeking Medical Attention
a. When to Consult a Doctor
Persistent and severe nausea and vomiting warrant quick medical attention. If women cannot keep food or liquids down, experience significant weight loss, or shows signs of dehydration such as dark urine, consulting a doctor is crucial.
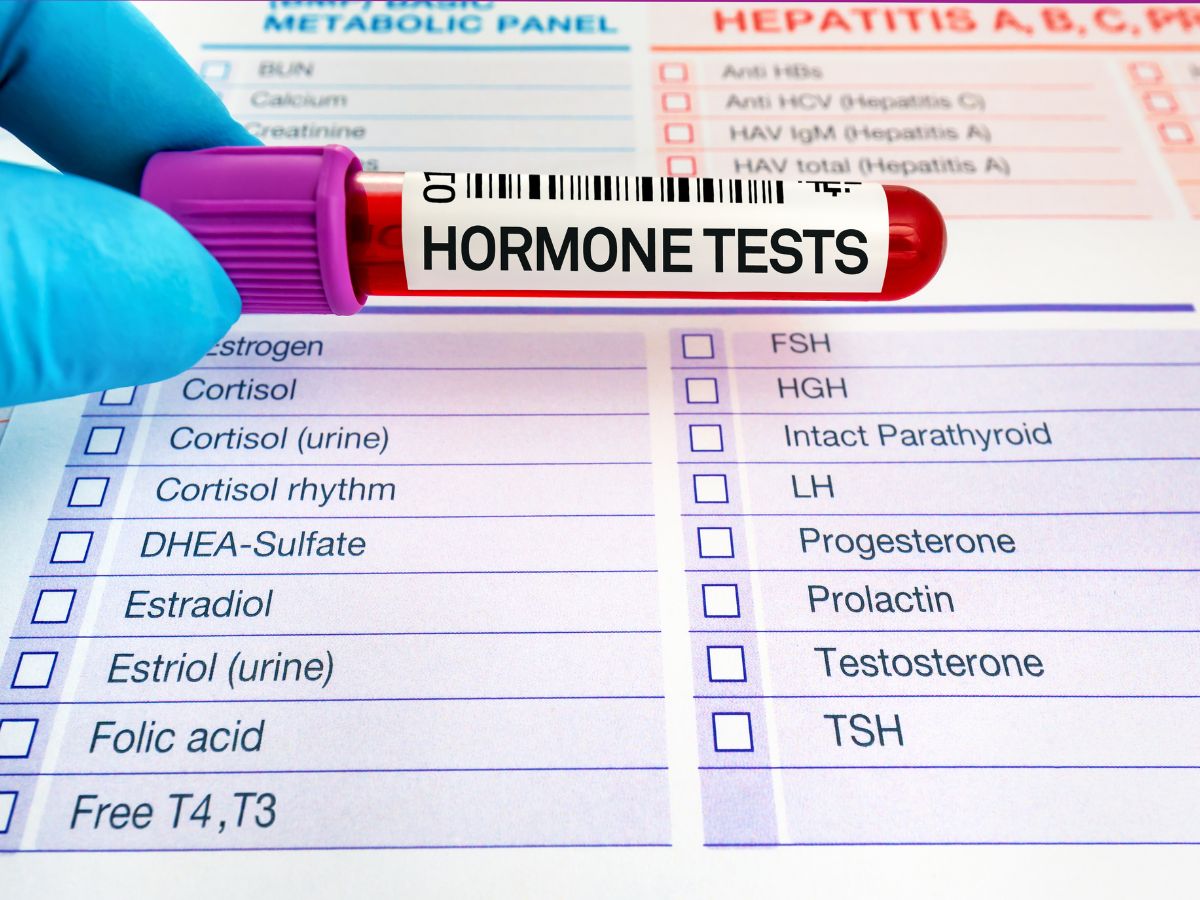
b. Diagnostic Procedures
Doctors may use various diagnostic procedures to assess the severity of symptoms and rule out other potential causes. These may include blood tests to check for dehydration and nutritional deficiencies, urine tests, and, in some cases, imaging studies to evaluate the patient’s overall health.
4. Management Strategies
a. Hydration and Nutritional Support
The cornerstone of HG management is addressing dehydration and nutritional deficiencies. Intravenous (IV) fluids may be administered to rehydrate the individual, and nutritional support through a feeding tube or intravenous feeding may be necessary to ensure nourishment.
b. Medications for Symptom Relief
Doctors can prescribe several medications to reduce nausea and vomiting in individuals suffering from HG. These may include antiemetics (medications to control nausea and vomiting), vitamin B6 supplements, and, in severe cases, corticosteroids to reduce inflammation.
5.Coping with Hyperemesis Gravidarum
a. Emotional Support
Dealing with HG is not only physically challenging but also emotionally taxing. Pregnant individuals with HG may benefit from emotional support, whether from doctors, support groups, or loved ones. Acknowledging the emotional toll and seeking assistance is crucial for overall well-being.
Also read: The Effects Of Maternal Hyperemesis Gravidarum On Fetus
b. Making Lifestyle Adjustments

Individuals with HG may need to make lifestyle adjustments to manage symptoms. This can include eating small, frequent meals, avoiding triggers that worsen nausea, and experimenting with different foods to find what is tolerable. Rest and stress management also play pivotal roles in symptom control.
6. Impact on Daily Life and Work
a. Navigating Work and Social Obligations
HG can significantly impact daily life, including work and social activities. Individuals with HG must communicate with their employers and peers, explaining the condition and potential limitations. Flexible work arrangements and understanding from others can contribute to a more manageable experience.
b. Balancing Self-Care and Responsibilities

Juggling self-care and daily responsibilities can be challenging for individuals with HG. Establishing a balance that prioritizes well-being while meeting essential obligations requires open communication with partners, family members, and employers to create a supportive environment.
7. Hyperemesis Gravidarum: Looking Toward the Future
a. Impact on Pregnancy and Fetal Development
While HG can be physically and emotionally taxing, most individuals with proper medical care can manage symptoms and continue with a healthy pregnancy. Adequate hydration, nutritional support, and medications can contribute to a positive outcome for both the pregnant individual and the developing fetus.
b. Counselling and Support Post-Pregnancy
The impact of HG may extend beyond the pregnancy, and individuals may benefit from counselling and support postpartum. Addressing any lingering emotional challenges and adjusting to life with a newborn can contribute to a more positive post-pregnancy experience.
Hyperemesis Gravidarum poses unique challenges for pregnant individuals, requiring a comprehensive approach to management and care. By understanding the causes, and symptoms, seeking quick medical attention, and implementing coping strategies, individuals with HG can navigate this challenging condition with resilience and support. This will also ensure the best possible outcome for themselves and their growing families.
