Share This Article
Postpartum depression and substance abuse pose complex challenges for new mothers. This article looks into the relationship between these issues, exploring their impact and potential coping mechanisms.
Postpartum depression, a complex mental health condition that can occur after childbirth, often presents a challenging and vulnerable period for new mothers. When coupled with substance abuse, the situation becomes even more tricky and dangerous. This dual struggle is bad for the well-being of the mother but also poses risks to the newborn’s development and the overall dynamics of the family. The intersection of postpartum depression and substance abuse emphasizes the necessity for comprehensive care and support. This includes both mental health treatment and addiction recovery services. Through understanding the triggers and underlying factors contributing to this dual diagnosis, this article aims to discuss effective strategies for treatment and recovery. It also emphasizes the importance of holistic and compassionate care to support mothers through this challenging phase.
1. Understanding Postpartum Depression
a. Defining Postpartum Depression
Postpartum Depression (PPD) is a mood disorder that affects mothers after childbirth. It involves persistent feelings of sadness, anxiety, and exhaustion, often hindering the ability to perform daily tasks and care for oneself and the baby.
b. Recognizing the Symptoms

Symptoms of PPD vary but may include persistent sadness, changes in sleep and appetite, feelings of worthlessness, and difficulty bonding with the baby. It is crucial to recognize these signs early for effective intervention.
Also read: Understanding Risk Factors for Postpartum Depression
2. Exploring Substance Abuse in the Postpartum Period
a. Defining Substance Abuse
Substance abuse involves the harmful or hazardous use of psychoactive substances, including alcohol and illicit drugs. In the postpartum period, women may turn to substances as a coping mechanism for the stressors and emotional challenges they face.
b. Identifying Risk Factors

Postpartum substance abuse is influenced by various factors. This includes a history of substance abuse, mental health issues, lack of social support, and the stressors associated with new motherhood. Identifying these risk factors is essential for preventive measures.
3. The Interconnected Challenge: Postpartum Depression and Substance Abuse
a. Understanding the Link
Postpartum depression and substance abuse often co-occur, creating a challenging cycle. Mothers may use substances to self-medicate PPD symptoms, aggravating mental health issues and leading to a harmful cycle that affects both the mother and the child.
b. Impact on Mother and Child

The interconnected challenges have significant consequences. Substance abuse compounds the emotional toll of PPD, hindering effective parenting and potentially leading to neglect or abuse. The child may face developmental issues and an increased risk of substance abuse later in life.
4. Risk Factors and Vulnerabilities
a. Common Risk Factors
Shared risk factors for both postpartum depression and substance abuse include:
- A history of trauma,
- Lack of a strong support system,
- Financial stress,
- The stigma associated with seeking help.
Recognizing these factors is crucial for tailored intervention.
b. Vicious Cycle of Self-Medication

Mothers with PPD may turn to substances as a form of self-medication, hoping to reduce emotional pain. This temporary relief can lead to dependency, intensifying mental health struggles and creating a cycle that requires specialized treatment.
Also read: The Impact Of Recreational Drugs On Fertility
5. Coping Mechanisms and Treatment Approaches
a. Counselling and Therapy
Combating postpartum depression and substance abuse often requires professional help. Counselling and therapy, both individual and group-based, provide a safe space for mothers to explore their emotions, develop coping strategies, and address the root causes.
Also read: Stigma Around Postpartum Depression: Maternal Mental Health
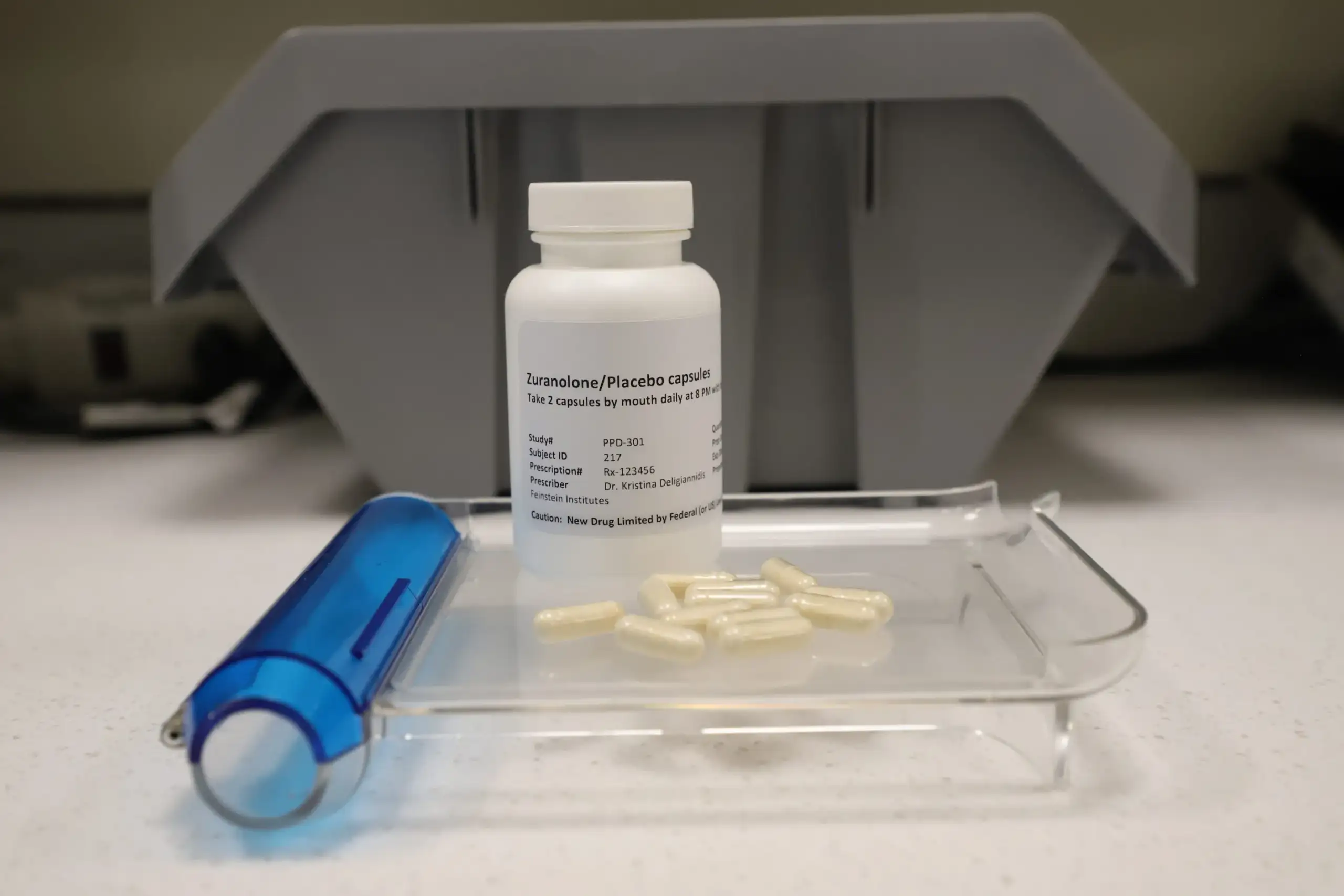
b. Pharmacological Interventions

In some cases, medication may be necessary. Prescribing medication for mothers coping with both postpartum depression and substance abuse demands a careful, individualized approach. This approach aims to avoid potential interactions or dependence on medications.
6. Preventive Measures and Support Systems
a. Education and Awareness
Preventing the dual challenges of postpartum depression and substance abuse starts with education and awareness. Doctors must inform mothers about the risks, symptoms, and available support systems during prenatal and postpartum care.
b. Building a Strong Support Network

A strong support network is critical. Family, friends, and community resources play an important role in helping mothers navigate these challenges. Reducing the stigma surrounding mental health and substance abuse encourages open conversations and seeking help.
Also read: The Importance Of Community Support In Postpartum Depression
7. Recovery and Moving Forward
a. Holistic Approaches to Recovery
Recovery involves holistic approaches addressing both mental health and substance abuse. Integrating therapies, support groups, and lifestyle changes promotes a comprehensive recovery plan that considers the unique needs of each mother.
b. Emphasizing Long-Term Well-being

Postpartum depression and substance abuse recovery is not a quick fix but a journey toward long-term well-being. Encouraging ongoing mental health support and addressing any relapse risks contribute to sustained recovery.
Postpartum depression and substance abuse demand a compassionate and tailored approach. By understanding the interconnected challenges, and risk factors, and promoting preventive measures, we can create a supportive environment that empowers mothers to navigate these dual struggles.